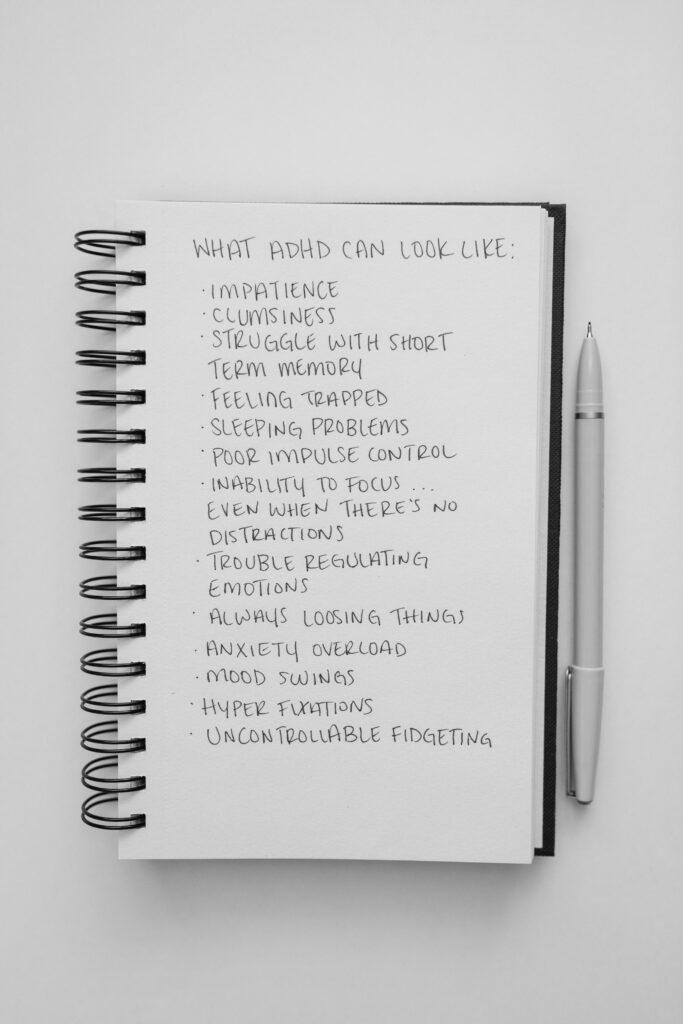
- Attention-Deficit/Hyperactivity Disorder (AD/HD) and Obsessive Compulsive-Disorder (OCD) although each different on their own, share certain common characteristics which can coexist due to overlapping genetic and neurological factors (associated with dysfunction in prefrontal cortex).
This coexistence can result in unique set of challenges for individuals, which I will be talking about here. Please note that for the purposes of this blog I am not discussing other possible conditions that present with similar symptoms or comorbidity (eg: autism, complex PTSD, chronic stress and burn out).
It’s estimated that up to 30% of those with OCD also have AD/HD, while around 20% of people with ADHD may experience OCD. It is note worthy to know that studies suggest 17 to 37% of individuals with autism also meet diagnostic criteria for OCD, compared to a 1-2% prevalence of OCD in the general population. Hence, whenever I have a client who presents with symptoms of either OCD, AD/HD or Autism, I get curious about the possibility of the other condition(s) being present.
Understanding this overlap, and distinguishing the symptoms associated with each condition can help choose and guide the right therapy and treatment modality on a case by case basis; as not one size fits all.
Similarities Between AD/HD & OCD:
Difficulty regulating thoughts and behaviours:
-
- AD/HD: individuals may struggle to filter out distracting thoughts and environmental stimuli due to dysregulated attention. Thoughts might at times be wandering, scattered, daydreaming, unfocused or spiral due to difficulty with controlling attention. Mental rumination can at times be triggered by emotionally charged events specially those triggering rejection or embarrassment (for example a conflict, or a social interaction). Mental rumination can present as replaying an embarrassing moment, a past event or planning future ones. All of this can result in distractibility, overstimulation, impulsivity or difficulty with decisions making.
-
- OCD: Obsessive and/or intrusive thoughts can cause very severe anxiety and feelings such as shame, guilt, or disgust which can result in one performing compulsions (mentally or behaviourally) in order to decrease the anxiety or discomfort. These thoughts can be very distressing, overwhelming and feel “sticky”. Which can cause repetitive thought cycling around the feared situation. For example: if one gets the intrusive thought of something bad happening to their parents they might have to undo that negative thought by thinking of a positive thought (to prevent that bad thing from happening, which can provide a momentary sense of relief).
Impact on Executive Function:
Given that the prefrontal cortex which is responsible for executive functions such as planning, organization, decision making, and impulse control is impacted in both AD/HD and OCD, individuals with either or both condition can struggle with this; but the underlying mechanisms, motivations and emotional impacts of each are different.
-
- AD/HD: Difficulty with procrastination (initiating tasks specially if there is no interest) and sustaining focus on task at hand. Individuals with AD/HD might be able to hyper focus on activities that are intrinsically interesting, stimulating, or rewarding (eg. hobbies, games, social media, creative projects). This, in combination with “time blindness” associated with AD/HD can result in one losing track of time, or struggle to redirect their attention to other priorities (contributing to both procrastination, and emotion dysregulation if forced to change direction).
-
- OCD: over focus on details, leading to perfectionism and difficulty with finishing tasks (which can look similar to AD/HD related hyper focus). When one is actively involved in acting out a compulsion it can be EXTREMELY difficult, frustrating and anxiety provoking for them if the compulsion is somehow disrupted or stopped. This can make shifting attention to another task very difficult. For example, if someone is actively counting (as a compulsion), and they are disrupted, this can cause extreme anxiety, the person might have the uncontrollable urge to complete the task fully before they can move on to something else. This can also result in tasks taking longer to complete, or things being done in a timely manner.
In short, in AD/HD the hyper focused behaviour is driven by interest or excitement but can result in lost productivity, while in OCD the behaviour feels necessary to relieve anxiety.
Emotion Dysregulation:
-
- AD/HD: emotions can be felt more strongly and deeply, due to multiple factors such as:
-
- Low dopamine activity which can affect mood regulation, making one more vulnerable to emotional extremes.
-
- Rejection Sensitive Dysphoria (RSD) is described as a heightened emotional response to actual or perceived rejection, criticism or failure. Studies suggest that children with AD/HD often receive more negative feedback from parents, teachers, and peers compared to their non-AD/HD counterparts. This increased exposure to criticism can significantly impact their emotional wellbeing and contribute to development of RSD. Stats suggest that approximately 50-60% of children with AD/HD experience rejection by their peers, compared to 13-16% observed in general elementary school populations (which can result in social isolation and impact social skills development). Thus, given the prolonged exposure to such negative interactions can result in trauma like responses in the brain/body when one is faced with minor criticisms or imagined slights, causing intense emotional pain or feelings of humiliation, anger or sadness. Subsequently, such feelings would be much more difficult for someone with AD/HD to manage and regulate when triggered, resulting in emotional reactions that seem disproportionate to the situation at hand.
-
- OCD: the emotional experience associated with OCD is VERY distressing to the individual and is usually associated with guilt, shame, disgust, fear, or something feeling wrong/immoral resulting in an urgent need to resolve or “fix” the thought. Not being able to act on, or complete a compulsion can result in EXTREME DISCOMFORT and anxiety, which can externally look like an angry outburst, agitation, or temper tantrums. Managing and regulating these emotions can be very difficult for the individual as these feelings are exacerbated by OCD symptoms.
Compulsive/Repetitive Behaviour:
-
- AD/HD: compulsive/repetitive behaviour could be a way of managing other symptoms such as forgetfulness, or emotion dysregulation. “Stimming” (short for self-stimulatory) are repetitive behaviours aimed to help one regulate their emotion or focus their attention (eg. fidgeting, pen clicking). Also, if someone is prone to losing things due to distractibility or forgetfulness as a symptom of AD/HD one might develop the comping mechanism of doing repetitive behaviour such as to check keys, wallet, doors/locks/appliances in order to avoid forgetting, losing things or to prevent making a careless mistake. This can then look like, or lead to OCD like checking.
-
- OCD: compulsions form as a response to an Obsession (a feared situation) or an intrusive thought in order to decrease the anxiety and discomfort brought in by the Obsession. For example: if someone gets the intrusive thought of having hit someone while driving, they might form the compulsion of going back and checking that they did not. Compulsions can also cause someone to repeat a ritual over and over, resulting in tasks taking longer to complete which can also look like perfectionism (for example: re-reading, re-writing texts, emails, home work).
Self-Doubt:
-
- AD/HD: the general struggles one experiences growing up with AD/HD can lead to repeated experiences of failure and criticism in academic, professional, and personal setting while living in a neurotypical society/environment that does not suit their brain and functioning. These negative experiences can over time lead to extreme self-doubt (Please visit the next post for more on ADHD and self-doubt).
-
- OCD: self-doubt can be a symptom caused by OCD. OCD HATES uncertainty; thus, obsessive thoughts can focus on “What if” scenarios, leading individuals to doubt their decisions, right/wrong or morality. Hence compulsions can form to mitigate the worst case scenario and bring in a perceived sense of control/safety all in the while reinforcing OCD. For example (excessive researching, reassurance seeking, checking with friends/family to make sure they made the right choice etc).
Social Justice Sensitivity vs right/wrong morality:
-
- AD/HD: individuals with AD/HD often show a heightened sense of fairness and justice, which is rooted in emotional sensitivity and empathy. Thus, they might react strongly to real or perceived injustices whether directed at themselves or others.
-
- OCD: “moral scrupulosity” is a subtype of OCD where the obsession is on moral or ethical correctness, driven by fear of making a mistake, causing harm or fear of the unknown/uncertainty.
When AD/HD & OCD Coexist:
- Exposure Response Prevention (ERP) for OCD
-
- AD/HD’s related impulsivity and forgetfulness or disorganization can clash with OCD’s need for control and perfectionism causing severe internal conflict, anxiety and can lead to feelings of failure.
-
- AD/HD’s related impulsivity can be followed by feelings of guilt which can be exacerbated by OCD related guilt, shame or anxiety over the consequences. For example: a symptom of AD/HD could be impulsively saying something out loud (not filtering), and with OCD there might be the fear (obsession) of hurting others (including emotionally). Hence, one with both AD/HD and OCD might be prone to both blurting something out, then experiencing extreme fear/shame, anxiety associated with the consequence of that, which can contribute to the formation of compulsions such as avoidance, checking (that did not hurt or offend someone), or mental rumination.
-
- AD/HD’s impulsivity and distractibility may lead to mistakes, while OCD’s obsessive tendencies can cause individuals to either ruminate on those errors endlessly, or increase procrastination/avoidant behaviour due to fear of consequence of making a mistake.
-
- Both conditions increase emotional sensitivity, making one more prone to self-critical thoughts, feelings of shame, inadequacy and doubt.
-
- Self-doubt and uncertainty can impact decision making, causing rumination, mental exhaustion and contribute to chronic stress.
Challenges of Co-Occurring AD/HD & OCD:
-
- Misdiagnosis: some AD/HD symptoms can mask OCD symptoms and vice versa; thus, the overlap and similarity in some of their presenting symptoms can result in misdiagnosing of one for the other. If not assessed in depth both AD/HD or OCD can be mistaken for other condition such as anxiety, or generalized anxiety.
-
- Medication: stimulant medications for ADHD can sometimes worsen OCD symptoms, and OCD medication is needed in higher doses in order to treat it properly; thus, correct diagnosis is required for the proper medication and dosage.
-
- Therapy: misdiagnosis can result in providing treatments that might not be a fit, or worst case scenario exacerbate certain symptoms. For example, if someone’s OCD compulsions is reassurance seeking, this can also show up in therapy. A knowledgable/skilled therapist would be able to recognize, assess, monitor and treat these symptoms appropriately using techniques such as what is provided by ERP, or ACT. General reassurance giving as means of decreasing client’s distress can contribute to exacerbation of symptoms or prolong suffering.
TREATMENTS:
Given the comorbidity between AD/HD and OCD, the combination of the two can result in a unique and confusing set of symptoms which require proper assessment and understanding. When AD/HD and OCD co-occur, best treatment should address both conditions. Having a proper assessment can go a long way in helping one not only learn about themselves and their brain, but to also find the tools, skills and a therapy modality, medication tailored to them and their needs.
Some treatments include:
-
- Exposure Response Prevention (ERP) for OCD & Acceptance and Commitment Therapy (ACT)
-
- AD/HD Coaching & CBT for AD/HD
-
- Strength Based & Creative Therapeutic Approaches such as Art or Expressive Therapies
-
- Family/Couples Therapy (as these conditions can impact families/relationships and dynamics)
-
- Medication
-
- Tailored Nutrition, Exercise & Supplementation
Book a free consultation with our team of experienced and knowledgable therapists today. Services offered in person in Vancouver, BC or Online